My name is John Newton. I’m 37 years old and this is the story of my battle with Meniere’s Disease. I have never written it down before and even when my father suggested I do so a few months back, I hesitated. I didn’t feel like writing at the time. These days, a re-aggravated back condition produces shaking in my hands and my ongoing dizziness often robs me of coordination. So spelling and grammar suffer a lot. Since I look at my keyboard to type, things get a wee bit wacky. Once again, before I exhaust my energy today, here’s “the rest of the story.”
PART TWO
October 20, 2012 — The Attack Sticks Around
After suffering through attacks of Meniere’s Disease for 11 years, I knew what would happen to my body each time and generally how long it would last. So whenever I woke up with roaring and ringing in my ears I knew that I needed to do several things:
- wear earplugs,
- turn off music,
- stay near walls, chairs and tables,
- and avoid typical headache triggers, like bright or flashing lights.
But I also knew that Meniere’s chose the time of its attack and not I. A few times it came the morning of a weekday, and I was affected at work. A few times it came on weekends, and I was affected in my other life pursuits. Sometimes it stayed for a week, one time for 24 hours. But one thing I knew for certain: it would go away eventually and always at night as I slept.
In October of 2012, however, I found myself one third of a world away, living in Edinburgh, Scotland and staying in the flat of new friends. That fall I decided to spend seven weeks living in Scotland’s capital to make personal connections, gather ministry ideas, and learn the culture of Edinburgh in preparation for a future ministry over there. It was an exciting and uncertain time. I had rented a car on the 15th of October and driven up to Inverness to pick up a ministry friend and then we went over to Aberdeen and then back to Edinburgh. On Saturday, the 20th, I planned a long road trip down to the Scottish Borders region and into Northeastern England. It was going to be a fun solo trip of exploration.
But on the morning of October 20th, I woke up with that familiar roaring and ringing in my ears. “Why now?” I pleaded with the sky. “Why here?” Again, Meniere’s picks the time. I don’t have a say. I wondered how the cold and humidity of Scotland (not to mention the wind) would affect this attack. Would it be worse? Would it somehow lead to further sickness? When I got up out of bed I could tell that my head was heavy again and my hearing was off. I did my usual routine of snapping, clapping and rubbing my fingers by my ears to determine how bad the hearing loss was this time. It wasn’t terrible, so I assumed I would be OK. The dizziness wasn’t bad, either. At least, I couldn’t tell while I was inside the cramped apartment.
 Since I was paying for the car by the day, and it wasn’t cheap, I knew that I had to use it. So I packed my things for the journey and gingerly made my way out of Edinburgh and into the Scottish countryside. I could tell that my balance wasn’t normal, but, somehow, driving on the left side of the road seemed to be kind of “correcting” the problem. I felt good as a driver, though the noise in my ears was louder than normal. I drove all around the countryside on narrow roads, hitting old ruin after ruin, crossing a tidal channel, visiting an island, and driving back to Edinburgh around dusk. It was a fun day overall and very educational. Minus the Meniere’s.
Since I was paying for the car by the day, and it wasn’t cheap, I knew that I had to use it. So I packed my things for the journey and gingerly made my way out of Edinburgh and into the Scottish countryside. I could tell that my balance wasn’t normal, but, somehow, driving on the left side of the road seemed to be kind of “correcting” the problem. I felt good as a driver, though the noise in my ears was louder than normal. I drove all around the countryside on narrow roads, hitting old ruin after ruin, crossing a tidal channel, visiting an island, and driving back to Edinburgh around dusk. It was a fun day overall and very educational. Minus the Meniere’s.
I had weeks left in Scotland so I assumed the Meniere’s attack would go away like it has before. After I turned the car in, I walked everywhere, up hills and down hills. It was great exercise and all but I got tired very quickly. By the time I had walked the mile from my room to Old Town Edinburgh, I was exhausted and needed to sit down. Thankfully, coffee shops are not uncommon in touristy Old Town, so I always had a place to regain my energy. As I have now learned, Meniere’s drains energy like teenage boys consume a pizza buffet. At the time I thought it strange that I was getting so tired. Before the Meniere’s attack I was strong-legged and walked up to five miles a day around Edinburgh. I found it invigorating. But during Meniere’s I struggled.
A few days passed, then a week and then… the Meniere’s attack remained. I waited and waited day after day for it to go away. Each night I would anticipate having the noise gone the next morning, only to awaken in frustration. By the time I left Scotland on November 15th, the Meniere’s attack had lasted nearly a month. And it wasn’t easing up. My head was heavy, I grew tired quickly, and sometimes (but not always) I found myself very off-balanced. I became thankful for street lamps, stone walls and railings. When I flew home I wondered how the airplane experience would affect my ears. Would the ear popping, you know, end me? Or at least make me scream in pain? I wore ear plugs the whole 11 hours through three flights without incident.
November 28, 2012 — Seeing a Specialist
My Meniere’s attack entered its sixth week before it was recommended by a friend to see a specialist at University of Texas Southwestern Medical Center in Dallas (UT-SW). My friend was a fellow Meniere’s sufferer and she said UT-SW had a really good Ear-Nose-Throat department. They do Meniere’s research, they told me. Since my condition wasn’t getting any better, and I had started to develop more serious balance issues since I got back from Scotland, I made an appointment. Thankfully, during five years of work at my church I had saved up more than $2,000 in an HSA account. Being without medical insurance ever since I became a missionary, that $2k was my salvation for getting help. So they connected me with a nurse practitioner who specializes in Meniere’s Disease research.
It was a very informative visit. I was first given an audio test to find hearing loss. The result was a loss in mid-range hearing primarily in my left ear. I was hearing impaired but not bad enough to warrant a hearing aid. The consultation with the nurse taught me even more. Here’s what I learned:
 Meniere’s (MnD) is being diagnosed more these days than it used to be. Over a million people suffer from it.
Meniere’s (MnD) is being diagnosed more these days than it used to be. Over a million people suffer from it.- MnD still has no known cause and no known cure. The nurse told me that there are many research reports on probable causes but no “smoking gun.” Some think MnD is caused by viruses, one even links it to the Herpes virus. Others suspect damage to the inner ear from a loud incident, like a rock concert or construction site. The jury is out on a cause. All scientists know is that MnD happens when the fluid of the inner ear is inflamed/agitated. And once it starts it usually calms but never seems to completely go away.
- More and more “triggers” that worsen attacks are being discovered. A trigger is something like, for example, bright light that makes a person dizzy. Other known triggers include salt, alcohol, changes in barometric pressure, allergies, lack of sleep, bending down (or over), reading and supermarket isles (I kid you not). I’m especially susceptible to lights, sleep loss, grocery stores, bending down, and reading. I think the grocery experience for me deals with light, noise, the beeping of the registers, turning my head to look left and right, and all the sensory information that has to be processed quickly. It makes me dizzy and exhausts me swiftly.
- The most recommended step a Meniere’s patient can take is to reduce sodium in the diet. A low-salt diet has given relief to some Meniere’s sufferers, the nurse said. It doesn’t affect noise in the ears, but it affects dizziness. She added an important caveat to this information: a low-salt diet doesn’t work for all Meniere’s patients. In fact, she had found no tangible research to indicate that body water and fluid in the inner ears is related. “It’s sketchy science,” she told me. “But it’s always a good idea for your general health.” I have found that going low-salt does nothing for my condition. But a friend of mine has found some relief.
- There are a number of experimental treatments for Meniere’s disease that are intended to lessen certain symptoms, especially dizziness and head pressure/pain. Some of these treatments have a “50-percent” risk attached. In other words, if it doesn’t help you it will take away your hearing for good. My nurse didn’t recommend these options except as a last resort.
So here’s what we did for a month to treat my Meniere’s. I was given a diuretic to reduce my body water and a steroid to see if it reduced the inflammation in my inner ear. I was also instructed to reduce sodium, which I did. It was tough to keep to it around Christmastime but I did my best. The result was disappointing. My MnD symptoms remained. Even worse, though, the steroid and diuretic worked against each other to cause horrible stomach pain. One pill dried me out, the other cramped my dry stomach. It wasn’t fun.
Over Christmas I traveled with my family to see loved ones and the car rides were tough on me. Motion, in general, got worse for me. When I arrived someplace my head felt pretty beat up. Not fun.
May 2013 — The Altitude Experiment
I made a bold decision during the spring of 2013, one that I hoped would finally bring relief to my ongoing Meniere’s attack. After a few months of constant symptoms, I was resigned to the fact that Meniere’s wasn’t just “going away soon.” I still had a faint, thin hope that it would just leave me but I also knew that I needed to do something original to combat the disease. So I came up with a hypothesis. Nowhere in my study of MnD research had anyone postulated that air density and air pressure (other than barometric changes) might affect the inner ears. I knew the structure of the ear really well by then. People get ear infections when the middle ear, which is open to the mouth cavity, gets blocked up by fluid. I knew that the ear drum was affected by air pressure. So what would happen if I lessened the air pressure on both my ear drum AND my middle ear? What if I did this for an extended period of time? Would it affect the self-contained inner ear?
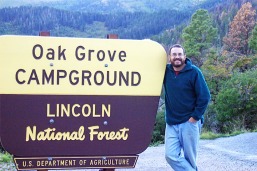 It was just a hypothesis but every hypothesis needs testing. So I decided to seek a higher altitude, less-humid climate than my native north Texas for the summer of 2013. I bought a pop-up camper, found a volunteer job with the Forest Service and moved to Ruidoso, New Mexico to run a public campground. The altitude at the campground was 8,400 feet. The humidity before monsoon season was 15- to 20-percent. I felt my ears pop as I climbed up to that altitude (which brought on dizziness) but once I arrived I knew that, regardless of my ears, I made a good decision to escape the Texas summer. It was 78 degrees when I arrived the afternoon of June 7th.
It was just a hypothesis but every hypothesis needs testing. So I decided to seek a higher altitude, less-humid climate than my native north Texas for the summer of 2013. I bought a pop-up camper, found a volunteer job with the Forest Service and moved to Ruidoso, New Mexico to run a public campground. The altitude at the campground was 8,400 feet. The humidity before monsoon season was 15- to 20-percent. I felt my ears pop as I climbed up to that altitude (which brought on dizziness) but once I arrived I knew that, regardless of my ears, I made a good decision to escape the Texas summer. It was 78 degrees when I arrived the afternoon of June 7th.
Here’s a summary of my stay as it relates to my MnD. I stayed in the altitude for four months until the government shutdown chased me out. During those months my dizziness lessened considerably, my energy was better, my head felt lighter, and I finally got some form of relief from my symptoms. I still had the noise in my ears, noise that forced me to wear ear plugs at night and lose a few hours of sleep, but that was the worst of my Meniere’s. Now, I must add that I did have spells every now and again. Often they were caused by some of the “triggers” I listed above. But I recovered from the spells faster in the altitude.
When I returned to the heavier Texas air in the fall, my condition became worse again. In fact, as I drove home, my head got heavier and my dizziness increased with every 500 feet of elevation I dropped. The last 90 miles of driving were some of the hardest I have ever experienced. But I had to get home!
January 2014 — “Stage Four” Commences
December ended on a pretty high note for me, personally. On the 29th I guest preached at a local church and stood the whole time without falling over (which was great). But after I had lunch with a friend the next day I started to feel sick. On New Years the flu had be down for the count. The first week of January I was very sick and by the time the 6th rolled around I started to realize something else was wrong with me. I was very weak, very dizzy and my head was always hurting. The roaring in my left ear had dialed up a notch, too, and not only was it roaring, it was also ringing. Now both ears were ringing!
 The flu eventually went away but I realized that my Meniere’s Disease had entered a new phase. I had no way to describe it to people, so I started calling it “Stage Four” of Meniere’s Disease. If Stages One and Two involved annual attacks, Stage Three was constant noise and more frequent spells, then Stage Four was constant noise, constant spells, sharp daily headaches and severe disability. For the rest of the month of January, I was a mess. I could not sleep, I could not work, I could not drive, I could not walk without walls close by. I have never felt so helpless! I remembered my conversation with the nurse at UT-SW back in 2012 and how she told me there wasn’t much they could do outside of experimentation and the pills I had already tried. So I had very little hope. It was dark. It was tough.
The flu eventually went away but I realized that my Meniere’s Disease had entered a new phase. I had no way to describe it to people, so I started calling it “Stage Four” of Meniere’s Disease. If Stages One and Two involved annual attacks, Stage Three was constant noise and more frequent spells, then Stage Four was constant noise, constant spells, sharp daily headaches and severe disability. For the rest of the month of January, I was a mess. I could not sleep, I could not work, I could not drive, I could not walk without walls close by. I have never felt so helpless! I remembered my conversation with the nurse at UT-SW back in 2012 and how she told me there wasn’t much they could do outside of experimentation and the pills I had already tried. So I had very little hope. It was dark. It was tough.
All during this “Stage Three” I had kindhearted people come up to me at church or I heard of them through family and friends and they would tell me, “Oh, my friend’s brother has that.” Or “my sister has it.” Then they would follow, “They’re much better now.” I know they meant very well and I appreciated their attempt to give me hope. I ALSO knew that the majority of Meniere’s sufferers were like I was for 11 years — once a year or occasional attacks that are manageable. They often go years between attacks. I long for those days now. Through my online research, I discovered that some 80- to 90-percent of Meniere’s patients do not have constant symptoms. And, like I once experienced, they come and go without warning. Indeed, I had now entered a “stage” that few ever reach.
February 2014 — A New Hope
In February, one of my parents suggested I at least try something new — to not give up but to fight. So I took to the internet to find alternative medicines, holistic treatments, and whatever advice I could get from other Meniere’s patients. I went on different forums and saw a kazillion suspected causes of Meniere’s and a kazillion treatments that worked for somebody. One alternative treatment seemed to stand out above the rest. It was developed by a MnD sufferer in Ohio and it tackled each symptom with either a vitamin or natural supplement. Called the “John of Ohio Regimen,” it seemed to be the most successful alternative to prescription medicine. “I need to do something,” I thought. “What harm is this going to do? If anything it’ll just add vitamins to my system and that’s not bad, right?”
I saw that the regimen called for taking between 10 and 16 pills a day, some of which I knew I couldn’t get at my local Wal-Mart, so I decided to err on the side of caution and only take half of the regimen. Some supplements were intended to fight against potential (but not actual) viruses and prevent the spread of Meniere’s from one ear into the other. I already was affected in both ears, so I left those out. Another pill was only available in Europe, so I left that one out. In the end, here is what I took and why:
- Vinpocetine, an extract of the periwinkle plant that is used in Europe for astronauts AND Meniere’s patients. It runs “interference” between your brain and your cocular nerve, helping your brain re-interpret the balance signals your ears are giving it.
- Lemon Bioflavanoid, an extract of the lemon rind, it strengthens capillaries in the inner ears, increasing blood flow to damaged areas in hopes of repairing the affected areas.
- Vitamin B2, also called Riboflavin, it is a natural substance found in foods (grains, especially) that also reduces the severity of head pain (I highly recommend this vitamin for headaches).
- Ginko Bilboa, a plant that also strengthens capillaries and improves brain function.
- Vitamin C, Extended Release, a common vitamin that, when released over time, works with the bioflavanoid and Vinpocetine on your inner ears.
I learned that the “John of Ohio Regimen” takes time to build up in your system, so I didn’t expect (or receive) immediate results. However, about a week later I started to feel better. First, the dizziness lessened. I would get dizzy going around corners and when driving but I would recover from my dizzy spells much quicker than before. Second, the head pressure was reduced to only pain that hindered me every-other-day and not every day. Third, as the weeks went on, I found myself able to read more without dizziness. And I actually started walking in a straight line — which was near impossible in January and February.
The month of March was very good. My Meniere’s was still with me and I had my bad days, but for the first time I had some hope. I thought that maybe I might be able to manage the worst of my symptoms.
April & May 2014 — A Call for Help
 My good run ended suddenly one Sunday morning in early April. I woke up feeling heavy headed and disoriented. When I took the supplements they had no effect. I was dizzy all day and miserable. The next day was more of the same, and then the next and so on. I was back where I was in January and the regimen no longer had any effect on me. Adding to the disappointment was an increase in the severity of my headaches. In early May I talked to a good friend and he suggested I contact UT-SW again. They were my only hope. So I set an appointment for May 12th.
My good run ended suddenly one Sunday morning in early April. I woke up feeling heavy headed and disoriented. When I took the supplements they had no effect. I was dizzy all day and miserable. The next day was more of the same, and then the next and so on. I was back where I was in January and the regimen no longer had any effect on me. Adding to the disappointment was an increase in the severity of my headaches. In early May I talked to a good friend and he suggested I contact UT-SW again. They were my only hope. So I set an appointment for May 12th.
I had another audio test and then met with the same nurse practitioner who saw me in 2012. She assumed I was doing better since I had not come back in 18 months (oops). She took my vitals and listened to my escalation of the disease. There had been some more research done into MnD since I last visited but no breakthroughs in curing the disease. She was still recommending a low-salt diet. “Did we try a diuretic?” she asked. “Yep.” I replied. “And?” “Didn’t work. You also gave me a steroid.” “And?” “It did wonders for a rash I had on my foot but nothing for my Meniere’s.” She chuckled at my rash remark but said, “There’s one more thing we can try. It’s what we’re recommending for people with vertigo issues. It something called betahistine. A compound drug.” I asked her what the positive response rate was to betahistine and she said, “About 43-to 46-percent success in reducing vertigo.” “Seems low,” I quipped. “It’s the most successful drug for Meniere’s patients,” she responded. I groaned.
One thing for everyone to realize is that what works for one MnD sufferer doesn’t necessarily work for another. This goes from daily life routines to diets to prescription drugs. Forty-six percent is astronomical for a Meniere’s treatment. So I had her write me up a prescription. I also got a drug called nortriptylin to reduce my headaches. She wanted to see me in a month to check on my progress. I got the betahistine filled out ($60) and nortriptylin ($4). And I took each according to direction every day along with a <1500mg sodium diet.
I also had an MRI to see if there was some other cause of my symptoms, or something else causing them to be so severe.
June 2014 — The Update
I had good news and bad news for my UT-SW provider. I met with a different nurse this time, one who specialized in migraine headaches. The nortriptylin reduced my headaches by 80-percent. I knock out the other 20 with Vitamin B2 and tylenol. But the betahistine failed to make a dent in my dizziness. It was the best prescription option. Oh well. The MRI came back clear (thankfully). The failure of betahistine may have indicated one of two things:
- I am among the 54- to 56-percent who do not respond to betahistine, or
- I have permanent damage in my inner ears that cannot be fixed by drugs.
In order to diagnose the second option, I had an ENG (Audio-Vestibular) exam in July. I was told beforehand it would be painful and uncomfortable and last an hour. They built me up for nothing! Well, one part of it was horrible but the rest was easy. And I failed with flying colors! Oh my. Suddenly mysteries of my health started to unravel and my reactions to treatments made more sense. I then met with a doctor and we discussed my condition and potential next steps. First, here’s my diagnosis and what it means:
 My left ear is likely my main Meniere’s ear. It responded slowly to stimuli and I had more difficulty with eye movement to my left than to my right.
My left ear is likely my main Meniere’s ear. It responded slowly to stimuli and I had more difficulty with eye movement to my left than to my right.- My right ear is over-active and responds too quickly to stimuli. This is either because it is trying to make up for my under-performing left ear or it, too, is damaged.
- Because there is damage in my ears, the normal Meniere’s treatments, from that John of Ohio Regimen to the betahistine will not work any more. The damage is too severe.
- The reason the regimen stopped working was likely because the ongoing Meniere’s attack had finally hurt my ears beyond the point of the supplements’ effectiveness. My window of getting results from supplements has passed.
Dr. Kutz of UT-SW saw me after my ENG exam and recommended two things: first, that I continue to watch my diet (OK… I get it!) and second, that I try a steroid injection in both ears. he said it is safe and it involves a steroid foam injection through the ear drum and into the middle ear. Over time the foam gets absorbed by the inner ear. I would have to have several injections over time in order to have meaningful results. After that, we’ll continue to troubleshoot and try new things. he upped my nortriptylin to try and get rid of all my headache, though it has not worked as of now (August 21). I’m still using B2 and Tylenol on occasion.
August 2014 — The Latest
As of this writing, I am still partly disabled by my Meniere’s Disease. I live in my parents’ house, I cannot work a normal job and there are many days I cannot drive. I have had to completely re-organize my life and eliminate potential futures, from jobs to living situations. I write as much as I can but there are many days I shake and dizz too much to write. Every now and again I get out, which must be like parole to a prisoner, and I drive myself to the store. Last Saturday I had my best day in a month, and I drove the lengthy distance of eight miles. Usually, driving wears me out since I have to concentrate extra hard on other cars, absorb a lot of visual motion and I get bumped around pretty good in my truck.
Mornings are my worst time of day. I am dizziest and have a heavy head in the mornings. As a result, I have had to cancel any and all ambitions of doing anything in the morning. I am an afternoon only person thanks to my MnD, and that only when I feel well enough to do anything.
As for the steroid injections, I’m not able to afford them at the time. My $2k dollars of HSA money has run out and my insurance won’t cover my Meniere’s disease (it’s a pre-existing condition). Adding to my insult, I was rejected for Medicare a few months ago without explanation. I have reapplied. Right now I’m trying to explore other public funding so I can treat this disease. Until then I’m keeping my head up and trying to push forward the best I can while managing my symptoms the best I can. It hasn’t been a good year for me so far, but there are still four months to go! I know there is a “Stage 5” of Meniere’s out there but I am determined not to get there. Not gonna do it. Nope!
I am very thankful to God for every day I live. Meniere’s Disease is just a bump in my road. Others around me are suffering so much worse, so I don’t like to share much about my condition publicly. And I won’t. There is no self-pity with me. I’ll be fine regardless of what my body does. No worries! God is good all the time. I believe that He loves me and will care for me whatever future lies ahead. Though the earthly tent is fading away, the inner man is renewed day by day.
— John